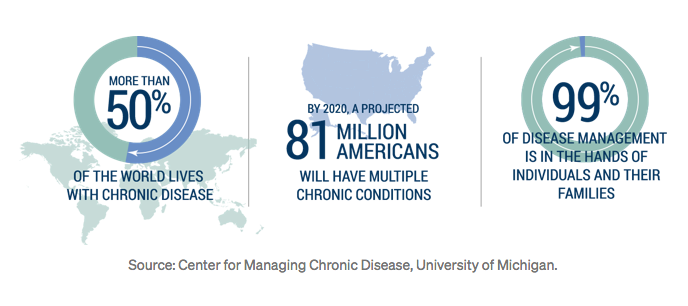
Chronic disease (e.g. diabetes, heart disease, respiratory disorders) affects approximately 50% of adults in the U.S., accounts for 86% of the $3.2 trillion U.S. healthcare spending, and is implicated in 7 of the 10 leading causes of death.
Chronic disease consumes 86% of the $3.2 trillion the U.S. spends each year on care
The current U.S. healthcare system cannot sustain the high cost and resource demand required to deal with the escalating caseload of chronic disease
The cost of treating preventable, chronic disease in the U.S. is almost 3 TIMES the combined purchase price of EVERY major sports league in the U.S!
This is primarily due to the fact that chronic diseases largely develop outside traditional healthcare surveillance. The healthcare community is finding that it’s best to think about chronic diseases as lifestyle-related diseases: afflictions arising from an individual’s lifestyle choices (e.g. activity, stress levels, diet).
Even the term healthcare is a misnomer because our current system is structured to treat disease on an emergent basis. Day-to-day monitoring of health and compliance with recommendations is not routine.
The true responsibility for chronic disease prevention and resolution currently rests with the patient. Lifestyle modification is no easy task. So, actually making a long-term commitment to lifestyle change has a low rate of compliance.
So how can we effectively change this situaition?
Enter Digital Therapeutics
Digital therapeutics are electronic devices that help people make positive and sustainable behavior change, yielding results that rival or surpass standard medication.
Digital therapeutics are mobile apps, wearable devices, and telemedicine platforms that complement or replace traditional therapeutics
Digital therapeutics don’t have the typical toxicity or associated side effects of traditional pharmaceuticals. In addition, this technology reaches the patient without the time and costs associated with regular visits to a hospital or doctor’s office.
Digital therapeutic programs achieve their high level of effectiveness by continuously monitoring patient vitals, while simultaneously encouraging and assessing compliance with recommended healthy lifestyle behaviors and prescribed medications. This paves the way for more opportunities to pair digital therapeutics with proven medicines.
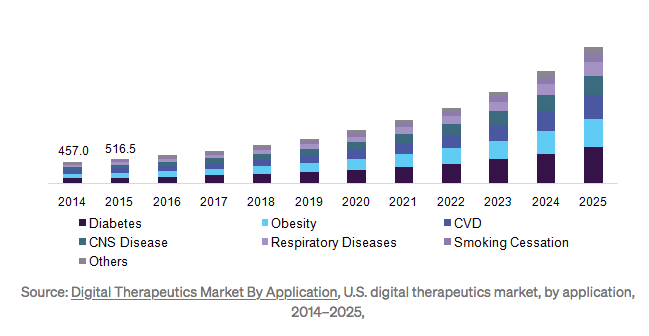
In recent years, the digital therapeutics space has been making great strides and growing quickly.
It is estimated that the market will reach upwards of $9B by 2025
A key differentiator for this category is its commitment to clinical validation and outcome-based reimbursement. We’ve listed a few notable milestones that have been accomplished thus far:
In June 2013, WellDoc launched the first FDA approved, digital prescription program, aiming to help diabetes patients manage their condition via mobile app.
In March 2016, the U.S. Department of Health and Human Services announced that it would reimburse digital therapeutic programs for administering the Diabetes Prevention Program (DPP), a lifestyle modification program, clinically proven to be more effective than drug alternatives.
In September 2017, the FDA approved a program developed by Pear Therapeutics, aimed at curbing substance abuse. This was the first prescription digital therapeutic with claims to improve clinical outcomes in a disease.
We believe this is just the beginning. These early players have set the stage and paved the way for incredible innovation in the space.The following are just a few of the established programs currently on the market:
Type 2 Diabetes Prevention/Management/Reversal (Omada Health, Blue Mesa Health, Canary Health, Virta Health) — extended programs promoting healthy habits and closely monitoring patient activity levels, diet, and weight, then pairing them with live health coaches, peer support groups, and/or clinicians. Early results have demonstrated that patients are not only capable of self-management, but could also "reverse” their condition without drugs or surgery.
Substance Abuse (Pear Therapeutics) — a prescription digital therapeutic used in conjunction with standard outpatient treatment for substance abuse disorder. As part of a traditional outpatient treatment program, this regimen has been clinically proven to increase abstinence from substance abuse and patient retention in treatment.
Asthma (Propeller Health) — partnered with GlaxoSmithKline to combine Glaxo’s asthma medications with a sensor-connected inhaler to monitor usage and provide biofeedback. Early results have demonstrated patients using the app require less medication over time.
Insomnia (Big Health) — utilizes visualization exercises to promote rest. Early results have demonstrated efficacy on par with sleeping pills and at a significantly lower cost.
Schizophrenia (Pear Therapeutics) — a prescription digital therapeutic to be taken in conjunction with medication.
ADHD, Major Depressive Disorder (MDD), Autism Spectrum Disorder (ASD) (Akili Interactive Labs) — delivering medicines through personalized, immersive video game experiences.
PTSD (Pear Therapeutics) — a prescription digital therapeutic that uses virtual reality-based simulation in conjunction with medication.
Heart Disease (Suggestic) — physician-approved, nutritional and lifestyle plans that guide patients to improved health states.
These advances are already being clinically implemented and improving lives. While we can’t say enough about them, we are also very excited about what’s to come.
Now, we'll ask three thought leaders on the front lines about what the future holds for digital therapeutics.
Q&A with The Experts
Curtis Duggan (@CurtisDuggan): CEO, Blue Mesa Health (@BlueMesaHealth)
Patty Mechael (@PattyMechael): Executive Vice President, Personal Connected Health Alliance (@PCHAlliance)
Adam Kaufman (@adambkaufman): CEO, Canary Health (@CanaryHealth)
1. BV: How would you describe the digital therapeutics space today?
Curtis: I would offer that digital therapeutics is at an inflection point in its journey through the hype cycle into a truly emerging new category of medicine. Reputable statistical summaries from the folks who aggregate funding data are showing record levels of funding but the volume of meaningful exits has not critically materialized. I think we are moving beyond the hype of 2010–2015, a cycle where a view, an erroneous view, I think, emerged — the concept that “apps” alone ipso facto could drive health outcomes.
I also think that digital therapeutics is emerging from the long shadow cast by the categorical definitions of Health IT and of for lack of a better term health infrastructure disruption. Digital therapeutics companies can often get lumped in with companies like Oscar, Clover and others. These notable health startups are taking big swings at the insurance problem, but they are fundamentally different from companies that are delivering repeatable outcomes.
There is still an enormous amount of education necessary to help distinguish the category from the umbrella of digital health writ large. Clearly there is funding, and there is buzz being directed towards the space.
Patty: What digital therapeutics represent, this concept of utilizing digital tools as an alternative to drug therapies or to improve treatment and enhance primary and secondary prevention efforts, is very exciting.
The field itself is still very nascent. While fragmented and poorly defined today, it’s an area of great opportunity that will continue to be galvanized and supported by its a focus on clinical validation at levels equivalent to traditional drugs and medical devices.
Adam: The idea of using digital technologies to drive patients toward better outcomes than traditional therapies alone (e.g. small molecules, biologics, medical devices) is incredibly compelling. The system has grown very comfortable with these established therapies and their underlying pathways, but we have turned a corner and are just beginning to see how digital tools can be utilized to enable people to be healthier.
2. BV: Do you feel the recent buzz surrounding the space warranted?
Curtis: Yes and no. I think there is probably too much buzz being directed towards the size of the funding rounds of a few companies, and not enough buzz on things that are being covered with less fervor because they are happening outside the Bay Area.
Where buzz is warranted is where companies are generating outcomes for their clients. I think we should focus less on funding rounds and more on whether companies are scaling towards a sustainable business model. Anyone can raise a hundred million dollars to pay personal trainers to follow people around eight hours a day and coach them on their habits in real time at a cost of twenty-thousand dollars per person annually and probably drive some excellent outcomes. But what are the unit economics?
I think we should focus on the overall global progress of the many hard-working companies who are building progress in the space and less on the size of a few venture rounds.
Patty: I do! I’m very excited about the personalization of health and health care experiences. Digital therapeutics enable the substitution, and in some cases enhancement, of drug therapies in a world where new approaches are needed and enable the healthcare system to engage patients more effectively. When people have the visibility into their own physiological processes and personalized guidance and tools to, they are able to take a more active role in their own care and self-management, we can keep more people healthy and out of the healthcare system.
Adam: This space is both underappreciated and overhyped at the same time; if you can believe it. It is underappreciated in the sense that we are just scratching the surface in terms of the profound impact digital tools will have on health. And it is overhyped in the sense that integration into our daily lives and within the healthcare system (e.g. workflow, regulatory/reimbursement pathways) will take time.
As Bill Gates surmised, we tend to overestimate the change that will occur in the next two years and underestimate the change that will occur in the next ten.
3. BV: In your view, what challenges/roadblocks lie ahead?
Curtis: I think the biggest challenges from a strategic point of view is educating the market to realize this “product” is not the proverbial ‘vitamin’, it is the ‘painkiller’.
All entrepreneurs and business strategists understand that the need-to-have pain-point-solver for a customer is always better than the nice-to-have. The digital therapeutics solution and effective, scalable prevention is a painkiller for a slow-moving pain.
Medicare is set to be overwhelmed by diabetes costs in the coming decade. Economic headlines coming out of the UK continue to sound the alarm that the NHS is about to becoming crippled by the skyrocketing costs of chronic disease. Health authorities and national governments in the Middle East and Gulf states are dealing with the burden of lifestyle-related disease as a key economic burden. This is an issue of national competitiveness.
However, as I have observed at the JP Morgan Healthcare Conference, the focus is still clearly on Stage IV Cancer treatments, end-stage renal disease dialysis innovation, rare diseases, genetic disorders and the like. This is life-saving work and it gets more attention because it is genuinely valuable life-saving work.
We have an opportunity to broaden the horizon of when we can intervene to save a life.
For a payer, intervention can happen earlier in the spectrum than when a patient is dealing with horrible chronic, acute and/or fatal diseases and it can happen in a way that is demonstrably cost-saving
Patty: Whenever there is too much hype, you run the risk of unwarranted backlash when a high- profile company or product doesn’t meet expectations. There is real potential here, and early efforts are demonstrating this, but we must be sure to keep the bar set high, particularly when it comes to evidence, and not be clouded by the hype. The FDA and evidence-based reimbursement pathways are actually helping with this.
Adam: I see identification of viable business models as the main challenge that newcomers face in the space. With traditional therapies, there is a relatively defined pathway to get reimbursed for devices or services. With digital therapeutics on other hand, companies must largely craft these models from scratch — there is no playbook. That said, in recent years, it has become less of a blank canvas as well, with early players in the digital therapeutics space having trail blazed a path to reimbursement that others can partially emulate.
4. BV: Paint us a vision of the future. How do you envision the healthcare industry and digital therapeutics space evolving over the next 5 years? 10 years?
Curtis: I believe that over the next five years we will see a consolidation of the companies that are actually delivering results and a culling of the herd where the emperor has no clothes (i.e. the company does not drive outcomes).
I think the last five years has been dominated by conversations around the ACA, insurance, access, coverage, political legislation, and policy. This is an important conversation, but I think we will see a shift towards coverage of more fundamental concepts of prevention and bending the overall cost curve.
I have political opinions on policy about the extent to which the state vs. private industry vs. the individual consumer should be responsible for health care costs.
However, that conversation rests atop a fundamental concept that, whoever is paying, to the extent that the population is healthier that payer is going save billions on costs
Look at what we’ve done in the last ten years. Ten years from now I think we will truly see a fundamental shift. Computing will change and we are likely to be using hands-free voice and AR to interact with the world. AI is overhyped right now, but in ten years we are likely to have digital therapeutics that are supercharged Siri or Cortana armed with volumes of data collected non-invasively through wearables.
We will have non-invasive glucose monitoring. We will be using the personal genome to sequence highly tailored personal medicine. I am bullish on Magic Leap, Hololens and the like and believe they can play a part in the future of digital therapeutics and population health. Frankly, I think mixed reality computing will all make us healthier because we will be interacting less with our screens and more with objects that sit naturally in physical space.
That’s how homo sapiens is meant to interact with physical space. I believe a key theme of the 2020s will be about the global shift in consciousness towards the eradication of all the drivers of chronic disease and mental illness.
Patty: Today, the healthcare ecosystem is still trying to figure out what the role of digital is for a particular condition or treatment course.
Over time, digital therapeutics will become seamlessly integrated with most health-related activities that put people at the center of their own care, enabling a coordinated care effort alongside remote monitoring and self-management
In a world where the list of drug side effects has begun to eclipse the list of health benefits, there is potential for effective digital therapies to eventually become the standard of care.
Adam: 5 years ago, there was a real question of whether digital programs would become part of healthcare. Today, I believe there is no doubt that digital programs are a key element of healthcare. Forward thinking employers and health systems have already begun adoption. As we look years into the future, digital therapies will play a significant role — now, the question becomes whether you will receive it from an employer, a health plan, or will it be a service offered by providers. I expect to see the organization of the industry evolve to answer these questions along the way to making this a part of standard care.
5. BV: What are you working on? Explain the significance to the industry’s bigger picture.
Curtis: At Blue Mesa Health, we are focused on being the world leader in mobile-first and culturally diverse chronic disease prevention. We don’t believe that technology alone can drive outcomes built for office workers or retail workers in America is going to work for someone in rural Latin America, nor will it work for someone in a heavily urbanized Gulf country like Saudi Arabia or Kuwait.
At least one billion people observe Ramadan, a month of observed fasting. Is the same program that serves suburban-swelling manufacturing employees in Pennsylvania or Ohio going to serve observant Muslims worldwide? Probably not.
To answer your question, I think the bigger picture is global, and Blue Mesa is focused on the global diabetes problem as strongly on our radar for future exploration.
Patty: PCHAlliance is focused on making health and wellness an effortless part of daily life. Digital tools enable this. We are exploring different ways to leverage innovation and technology to guide individuals and personalize treatment to help them live longer, healthier lives.
In collaboration with the Consumer Technology Association (CTA) and Ipsos Healthcare, PCHAlliance has been researching the digital therapeutics landscape and aims to mobilize members to help define and advance this space further.
Adam: At Canary Health, we are working to place the individual back at the center of their own healthcare. Utilizing digital tools, Canary is developing personalized, self-management support programs for patients to use in complement with traditional healthcare settings. Our self-management technology is versatile and can be applied to many patient subgroups. We are currently exploring pre-diabetic care, and have aspirations to expand into additional chronic disease states, such as diabetes, heart disease and COPD.
6. BV: Anything else you would like to share or discuss that was not addressed above?
Curtis: The main thing I’d like to add is simply a call to people who might benefit from our program. We can talk about payers, providers, venture capitalists, macroeconomics trends, and epidemiology for hours.
In the end though, the biggest thing we want to do is let people know that there are great programs out there that actually work.
Summary
Instead of attacking the root cause of the healthcare crisis — the unhealthy behavior that leads to chronic disease — our system has chosen to instead focus on treating and masking the symptoms of these diseases.
There can be no solution to the healthcare crisis that does not address America’s unchecked epidemic of chronic disease.
Digital therapeutics aim to shift this way of thinking and instead tackle the underlying problem: patient behavior. It’s early in the game, but the data is starting to accumulate and the potential to enhance patient experience and outcomes is clear. Keep a close eye on this space — it’s just getting started.